What is Blood Cancer?
Blood cancer is a type of cancer that affects your blood, bone marrow, or lymphatic system. Unlike other cancers that form solid lumps or tumors (like breast or stomach cancer), blood cancer spreads through the body because blood flows everywhere.
Your blood has three major parts:
- Red blood cells (RBCs): Carry oxygen
- White blood cells (WBCs): Fight infections
- Platelets: Help stop bleeding by clotting blood
When someone has blood cancer, these cells don’t grow or work the way they should. The cancerous cells grow quickly and crowd out the healthy ones. This weakens your immune system, affects oxygen supply, and causes bleeding problems.
Types of Blood Cancer
Blood cancer is not just one disease—it includes different types, each with its own way of affecting the body. The main types are leukemia, lymphoma, and multiple myeloma. While all of them start in the blood or the tissues that make blood, they behave differently and need different treatments. Understanding these types can help you feel more informed and less overwhelmed.
1. Leukemia:
Leukemia is probably the most commonly heard of when people talk about blood cancer. It starts in the bone marrow, which is the soft, sponge-like tissue inside your bones. This is where your body makes new blood cells. In leukemia, the bone marrow starts making too many white blood cells, and these cells don’t work the way they should. These abnormal white cells grow fast and crowd out the healthy red blood cells, white blood cells, and platelets. As a result, the body struggles to fight infections, carry oxygen, and stop bleeding.
Leukemia can be either acute or chronic. “Acute” means the cancer develops and spreads very quickly, often within days or weeks. It needs immediate treatment. “Chronic” leukemia develops more slowly and may not cause symptoms right away. It can sometimes be managed for years.
2. Lymphoma:
Lymphoma starts in the lymphatic system. This system is a network of nodes and vessels in your body that helps you fight infections and filter out harmful substances. In lymphoma, a type of white blood cell called a lymphocyte turns cancerous and grows out of control. The lymphatic system runs throughout your body, so lymphoma can start almost anywhere—like the neck, chest, or groin. One of the early signs is usually painless swelling in the lymph nodes. It might be mistaken for a common infection at first, but if the swelling doesn’t go down, it should be checked by a doctor.
There are two main types of lymphoma: Hodgkin lymphoma and Non-Hodgkin lymphoma. Hodgkin lymphoma is curative, especially when diagnosed early. Non-Hodgkin lymphoma is more common and has many subtypes, each behaving differently. Some types grow very slowly and may not need treatment right away, while others are aggressive and need immediate care.
3. Multiple Myeloma:
Multiple myeloma is a different kind of blood cancer that affects plasma cells. These are a special type of white blood cell found in the bone marrow. Normally, plasma cells help your body fight infections by making antibodies. But in multiple myeloma, these cells become cancerous and start producing abnormal proteins that don’t help the body at all. These abnormal plasma cells build up in the bone marrow and take over the space meant for healthy blood cells. This can lead to many problems, like weak bones, anemia, frequent infections, and kidney damage.
One of the unique things about multiple myeloma is that it often causes bone pain, especially in the back or ribs. People may also feel very tired, experience frequent fevers, or notice bruising easily. This type of blood cancer can be long-lasting but is often manageable with treatment. Therapies may include medications that target the cancer cells, chemotherapy, stem cell transplant, and supportive care like bone-strengthening drugs or blood transfusions.
Risk Factors of Blood Cancer
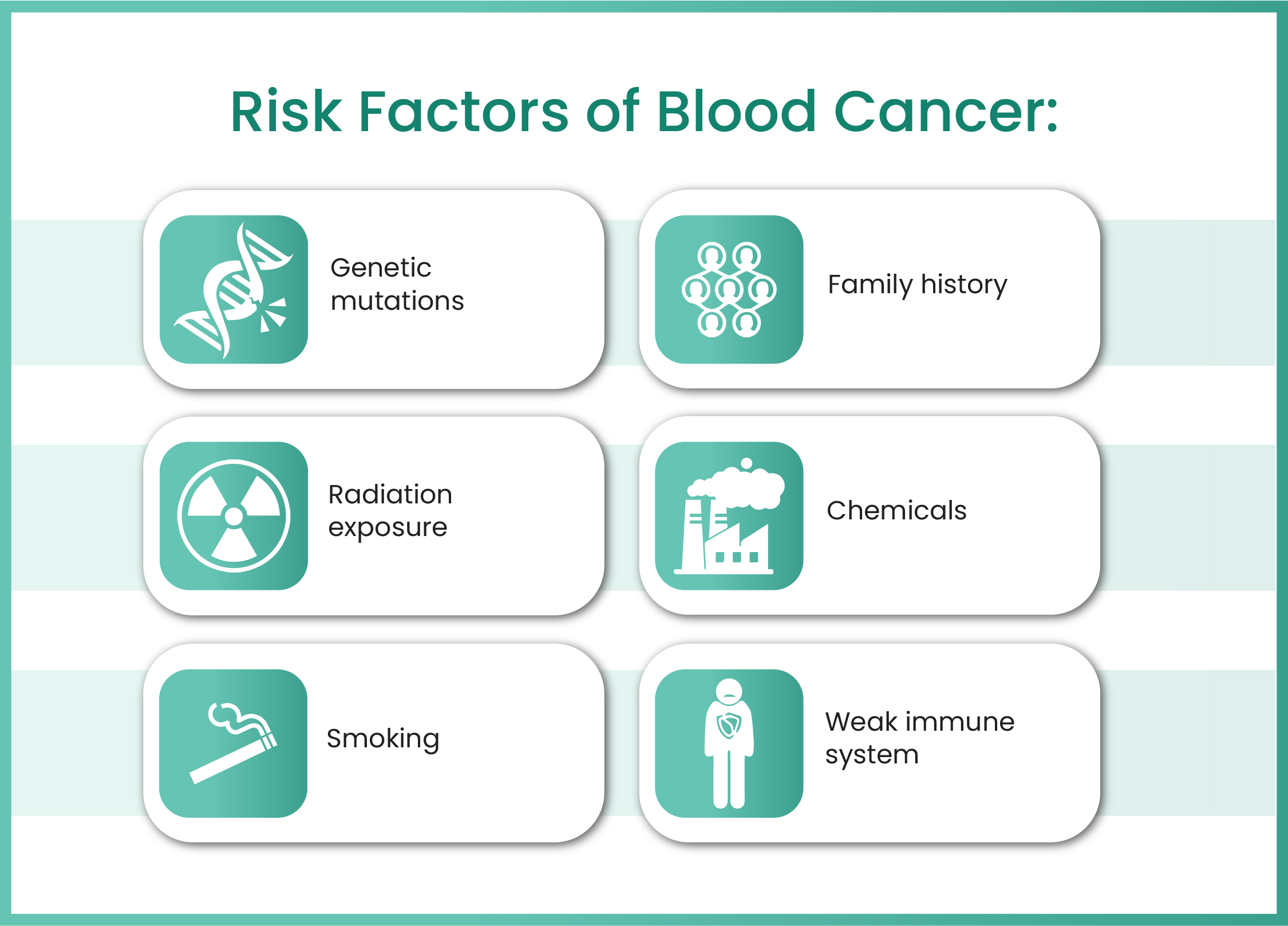
The exact cause of blood cancer isn’t always known. But several factors can increase the chances of developing it.
- Genetic mutations: Changes in DNA that affect how cells grow.
- Family history: If a close family member had blood cancer.
- Radiation exposure: Especially from past cancer treatments or nuclear exposure.
- Chemicals: Long-term exposure to chemicals like benzene.
- Smoking: Increases the risk of certain types of leukemia.
- Weak immune system: Such as from HIV/AIDS or after an organ transplant.
Just having a risk factor doesn’t mean you’ll get blood cancer. Many people with risk factors never get it, and some with no known risks do.
Signs and Symptoms of Blood Cancer
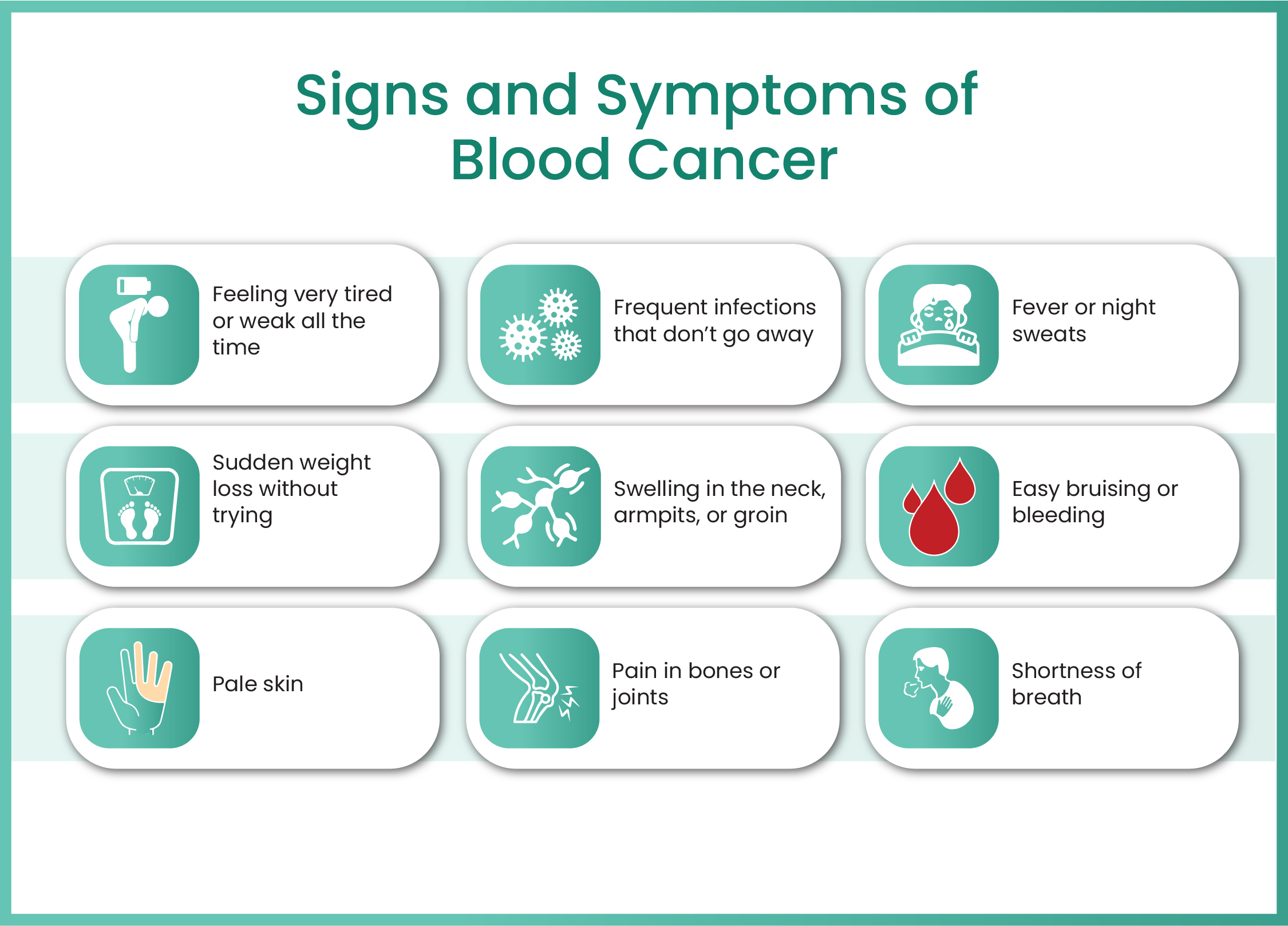
Blood cancer symptoms can look like common illnesses at first — such as tiredness or flu. But when they don’t go away or keep coming back, it’s time to check with a doctor.
- Feeling very tired or weak all the time
- Frequent infections that don’t go away
- Fever or night sweats
- Sudden weight loss without trying
- Swelling in the neck, armpits, or groin (swollen lymph nodes)
- Easy bruising or bleeding (nosebleeds, bleeding gums)
- Pain in bones or joints
- Pale skin
- Shortness of breath
How Blood Cancer is Diagnosed?
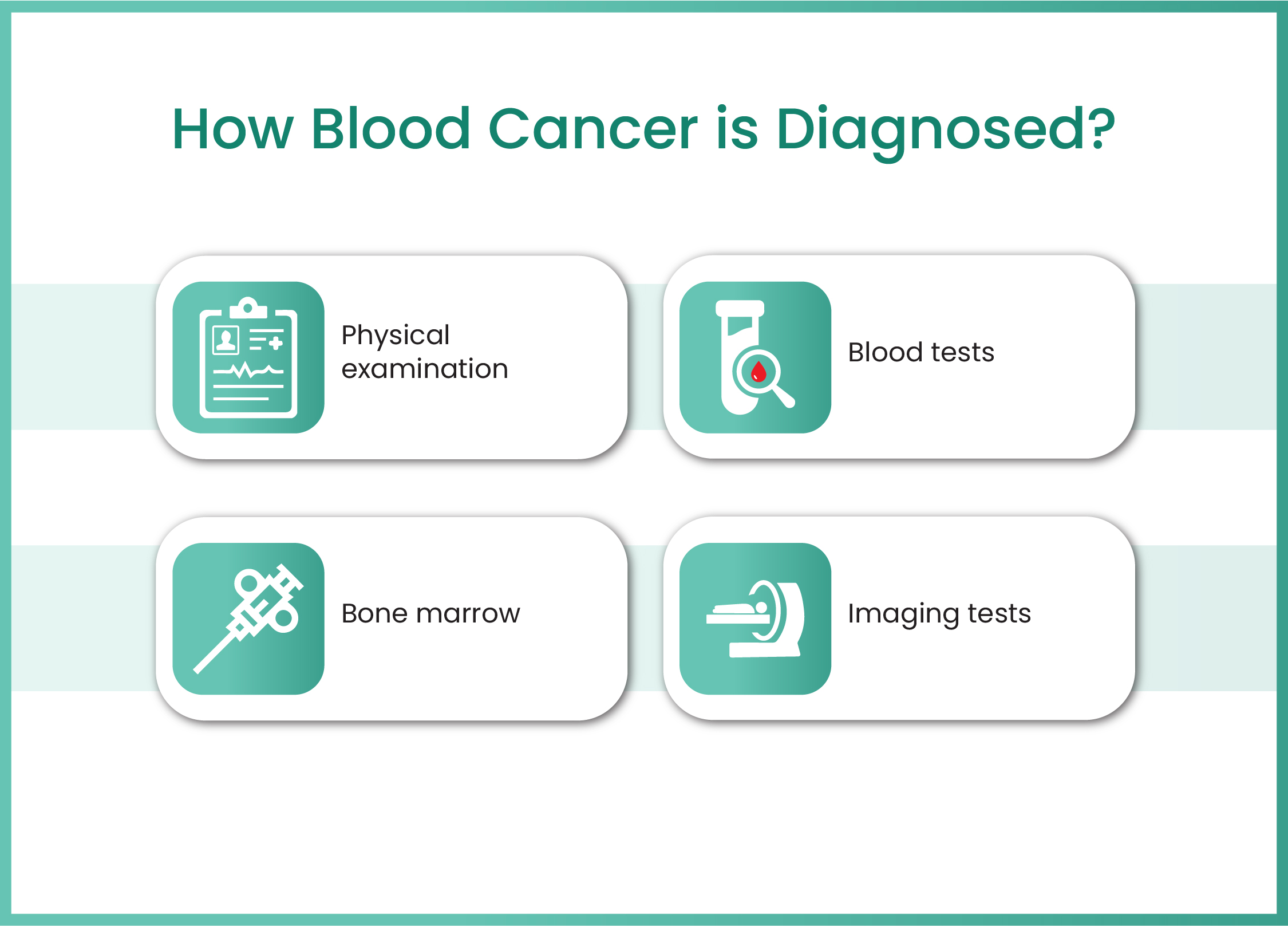
1. Physical examination: The first step often begins with a physical examination and a detailed discussion about how the patient has been feeling, what symptoms they’ve experienced, and whether there’s any family history of cancer or serious illness.
2. Blood tests: After this initial consultation, the doctor usually recommends a set of blood tests. One of the most important ones is called a complete blood count (CBC). This test looks at the number and types of cells in your blood — including red blood cells, white blood cells, and platelets these are called as blasts cells. If there are too many or too few of any of these, or if the cells look abnormal, it can be a sign that something is wrong in the bone marrow where these cells are made.
3. Bone marrow/biopsy tests: If the blood test shows unusual results, the next step is to look more closely at the bone marrow — the soft, spongy tissue inside your bones. This is done through a bone marrow biopsy. During this test, a small sample of bone marrow is taken, usually from the hip bone, using a special needle. This might sound scary, but it’s a routine procedure and is done under local anesthesia so the patient doesn’t feel pain. The sample is then sent to a laboratory where it’s checked under a microscope to see if there are any cancer cells present. Special test like flow cytometry, cytogenetics and molecular tests are performed on the bone marrow samples. These tests helps for staging and prognosis.
4. Imaging tests: CT scans, PET scans, or MRIs are also used. These scans give doctors a detailed picture of what’s happening inside the body. For example, if a person has swollen lymph nodes or an enlarged spleen, these tests can help show how far the disease has spread. In some cases, especially if lymphoma is suspected, a lymph node biopsy may be done. This means removing a small part of a swollen lymph node and examining it to see if there are cancer cells in it. The imaging tests help for staging and monitoring the disease response.
Lifestyle Tips During and After Treatment
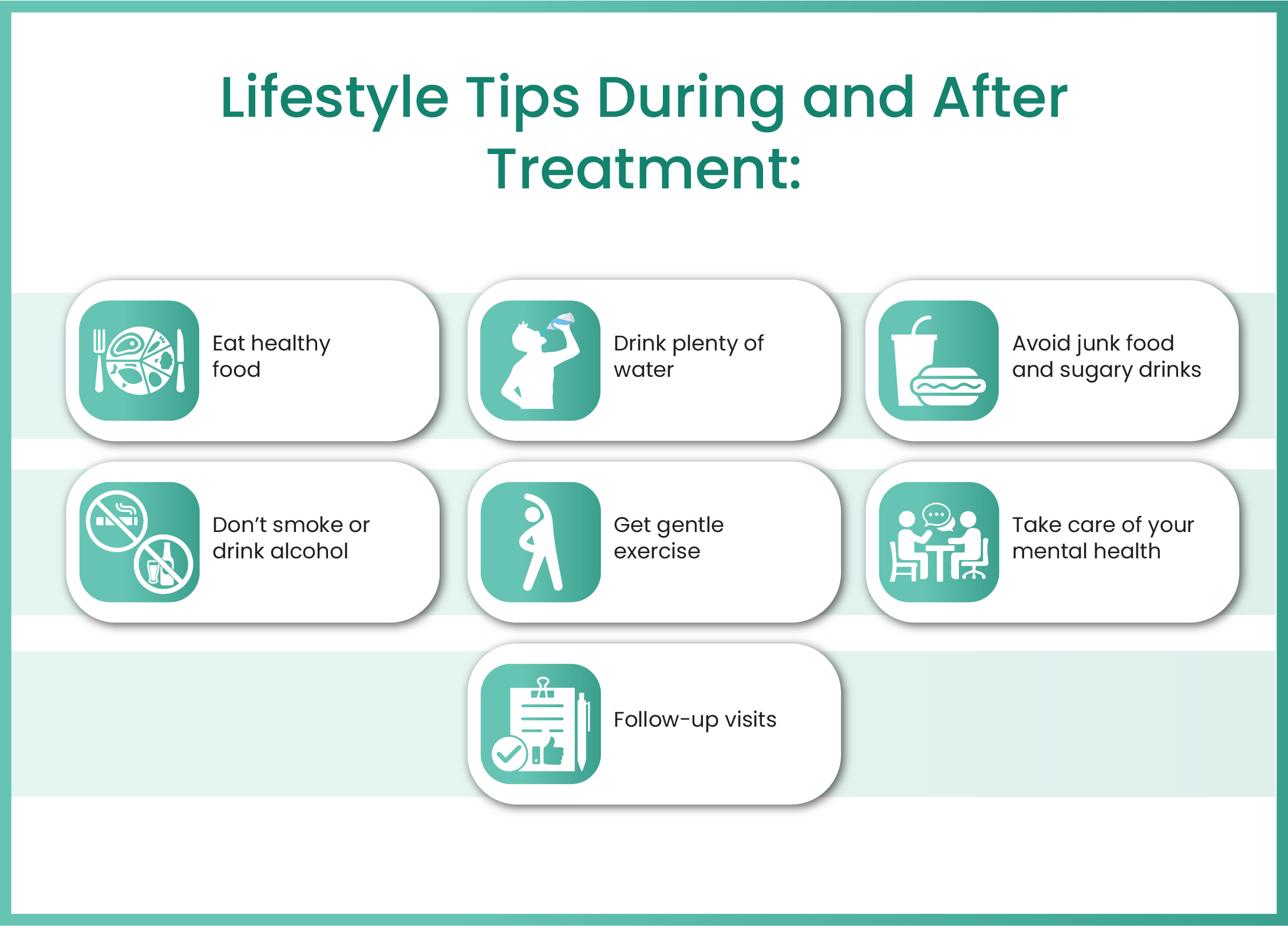
Fighting cancer isn’t just about medicines. Your lifestyle also plays a big role in how well you respond to treatment and how quickly you recover:
Helpful lifestyle changes:
- Eat healthy food: Include fruits, vegetables, lean protein, and whole grains.
- Drink plenty of water: Stay hydrated.
- Avoid junk food and sugary drinks.
- Don’t smoke or drink alcohol.
- Get gentle exercise: Like walking or light yoga to keep your energy up.
- Take care of your mental health: Talk to a counselor or join a support group.
- Follow-up visits: Never skip checkups — they help detect problems early.
Treatment Options for Blood Cancer
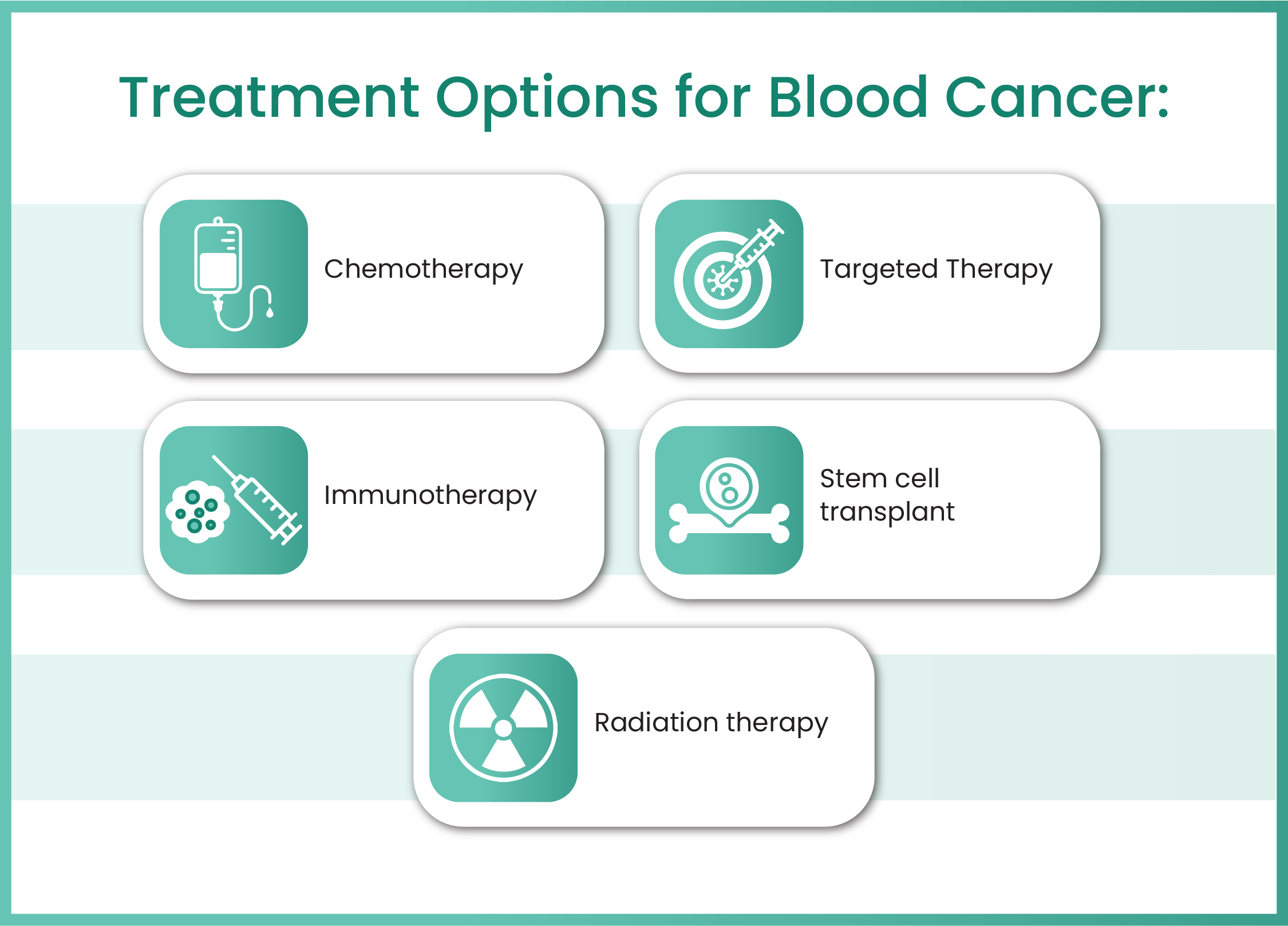
1. Chemotherapy: Chemotherapy uses strong medicines that travel through the bloodstream to reach and destroy cancer cells. These medicines are usually given through a drip (IV) or taken as pills. Chemotherapy works by targeting cells that grow quickly, which includes cancer cells. However, it can also affect some healthy cells, which is why people might feel side effects like hair loss, tiredness, or nausea. But many of these side effects can be managed with proper care, and they often go away after the treatment ends.
2. Targeted Therapy: This is a more advanced form of treatment that focuses only on the cancer cells and leaves the healthy ones alone. Targeted therapy looks for specific markers or changes in the cancer cells and uses special medicines to block those changes. Because it attacks only the bad cells, many people find it easier to tolerate than chemotherapy. It’s like sending a smart missile to destroy the enemy without damaging the surroundings.
3. Immunotherapy: This method helps the body’s own immune system fight the cancer. Normally, your immune system protects you from diseases. But in blood cancer, cancer cells can hide from your immune system or stop it from working properly. Immunotherapy boosts or trains your immune system to recognize and attack cancer cells more effectively.
4. Stem Cell Transplant: This is also known as a bone marrow transplant. In this treatment, the patient first receives high doses of chemotherapy (sometimes radiation too) to destroy all the cancer cells. Then, healthy stem cells are introduced into the body to rebuild the bone marrow and help it produce healthy blood cells again. These stem cells may come from the patient’s own body (collected earlier) or from a donor. It’s a complex procedure, but for many patients, it offers a chance at a complete cure.
5. Radiation Therapy: Radiation therapy is sometimes used in blood cancer treatment, especially in lymphoma. Radiation uses high-energy rays to target and kill cancer cells in specific parts of the body. If a patient has a large tumor or a swollen lymph node that’s causing problems, radiation can help shrink it quickly. It’s usually used along with other treatments like chemotherapy or after a transplant.
6. Cellular Therapy (CAR-T Cell Therapy / BiTE Therapy): This is one of the most promising and cutting-edge options for certain types of blood cancer.
- CAR-T Cell Therapy involves collecting a patient's T-cells (a type of immune cell), modifying them in a lab to recognize and attack cancer cells, and then infusing them back into the patient’s body. It’s highly personalized and has shown remarkable results in treating some leukemias and lymphomas.
- BiTE (Bispecific T-cell Engager) Therapy is another exciting innovation. It uses specially designed antibodies that bind both cancer cells and the patient’s T-cells, bringing them together to destroy the cancer cells directly.
Dr. Reetu Jain is a highly respected blood cancer specialist in Mumbai, known for her compassionate care, deep expertise, and personalized approach to treatment. With years of experience in managing complex cases of leukemia, lymphoma, and multiple myeloma, she is widely regarded as one of the best oncologist in Mumbai. Her dedication to patient care, combined with her use of the latest medical advancements—such as targeted therapy, immunotherapy, and stem cell transplants—makes her a trusted choice for families seeking reliable and effective cancer treatment. Patients often describe Dr. Reetu Jain not only as a skilled blood cancer doctor in Mumbai, but also as a comforting presence during one of the most difficult times in their lives.
Frequently Asked Questions (FAQs)
Yes, many types of blood cancer are curable, especially when diagnosed early. With today’s advanced treatments like chemotherapy, targeted therapy, and stem cell transplants, many patients go into complete remission. However, every case is different. Factors like the type of blood cancer, the stage at diagnosis, and the patient’s overall health all play a role
It’s a common and fair question. Blood cancer doesn’t always have a clear cause. While some cases are linked to genetics, radiation, or chemicals, many people develop it without any known risk factors. It’s not something you caused or could have prevented. Sometimes, random changes in the body’s cells lead to cancer. That’s why regular health checkups and awareness of symptoms are so important.
Yes, unfortunately, blood cancer can affect children as well. In fact, leukemia is one of the most common cancers in children. The good news is that children often respond very well to treatment. Pediatric oncologists work closely with families to provide child-friendly care and support throughout the journey.
Some types of blood cancer can come back, which is called a relapse. However, regular follow-up tests help doctors catch any changes early. If the cancer does return, there are still treatment options available. Many patients go into remission again after further care.
Absolutely. Eating healthy, staying hydrated, getting gentle exercise, and managing stress all help the body heal. Avoiding smoking and alcohol, taking medications on time, and following your doctor’s advice are also important


