Ovarian Cancer
Ovarian cancer often develops with subtle or no noticeable symptoms, making early detection challenging. By the time it whispers instead of shouts, it may already have spread beyond the ovaries. That is why clear, calm, and trustworthy information is essential. The goal of this page is simple: to explain everything about ovarian cancer in language that feels like talking to a caring friend. From risks and early warning signs to modern treatments and lifestyle tips.
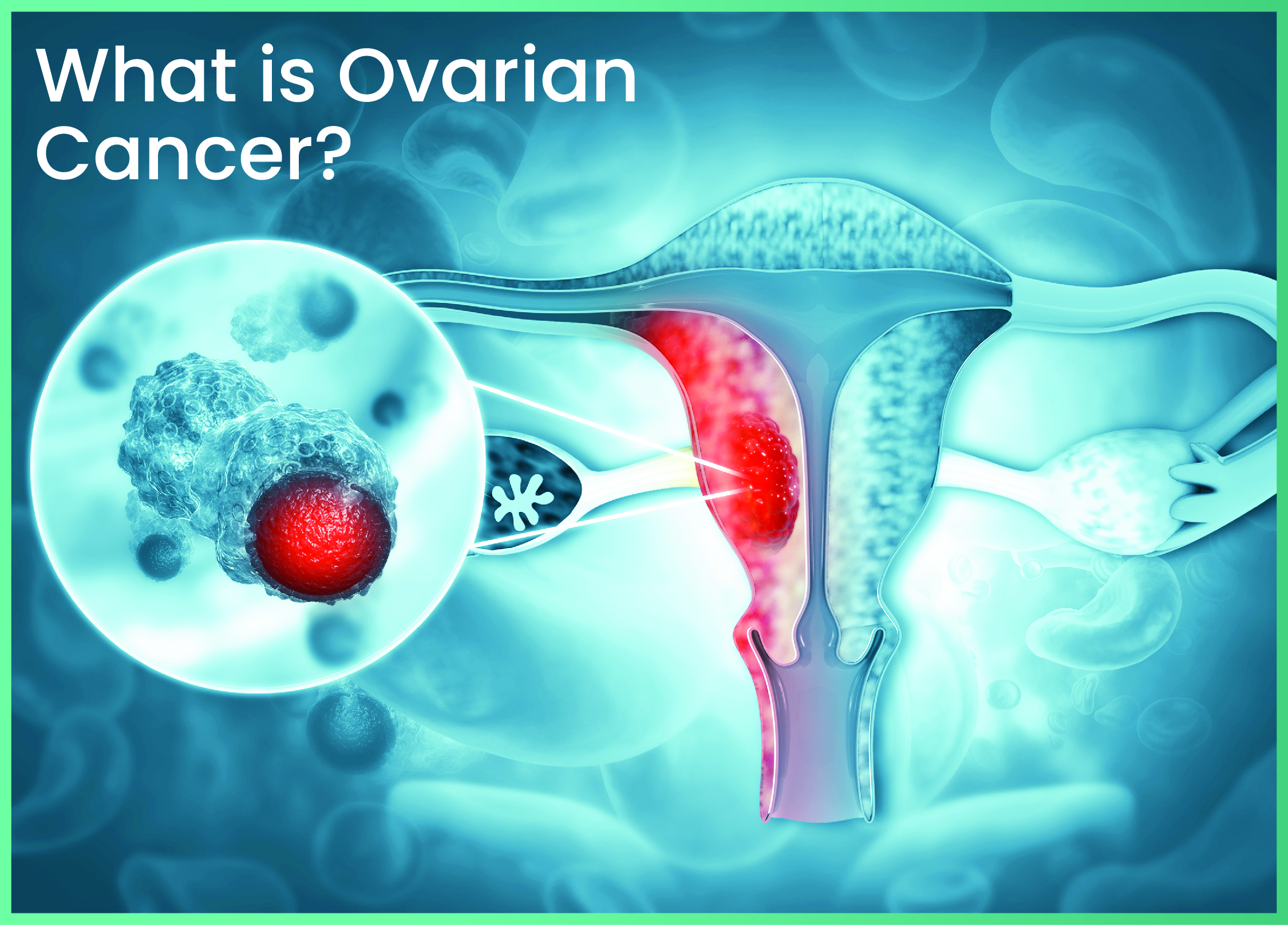
What is Ovarian Cancer?
Your ovaries are two small, almond-shaped organs tucked deep in the pelvis. They produce eggs and release hormones that guide the menstrual cycle, bone strength, and much more. Ovarian cancer develops when certain cells inside or on the surface of an ovary begin to grow out of control. Over time these rogue cells can form a tumour, break away, and travel through the abdomen or even the bloodstream.
Unlike some cancers linked to obvious lifestyle choices (such as smoking and lung cancer), ovarian cancer is more complicated. It results from a blend of age, genetics, hormonal factors, and plain biological chance. The good news? Advances in screening, surgery, and medication mean many women today live long and active lives after diagnosis — especially when guided by experts like Dr Reetu Jain, recognised as one of the best ovarian cancer doctors in Mumbai.
Types of Ovarian Cancer
Epithelial ovarian cancer
This type begins in the outer layer of cells that cover the ovary. These cancers usually happen in women over the age of 50 and are often diagnosed in later stages because they don’t cause clear symptoms in the beginning. Even within this category, there are several subtypes like serous, endometrioid, mucinous, and clear cell. Serous is the most common subtype and tends to grow more quickly. Endometrioid and mucinous types often grow more slowly and may have a better outlook if caught early. Clear cell cancer is less common but can be more aggressive.
Germ cell ovarian cancer
This type begins in the cells that produce the eggs in the ovaries. It mostly affects younger women and teenagers. These cancers are rarer but usually respond very well to treatment, especially if found early. Doctors can often treat them with surgery and chemotherapy, and in many cases, fertility can be preserved.
Stromal or sex cord-stromal tumors
These cancers grow from the tissues that support the ovary and help produce female hormones like estrogen and progesterone. One of the unique things about this type is that it often produces hormones, which can cause unusual symptoms such as abnormal bleeding or early puberty in young girls. These tumors usually grow slowly and are often diagnosed at an early stage.
Small cell ovarian cancers
These are uncommon and tend to be very aggressive. Because they are so rare, doctors often study them in research settings to better understand how to treat them.
Risk Factors You Should Know
Every woman is unique, but a few common threads tie many ovarian cancer cases together:
Age: Most diagnoses occur after menopause, usually between 50 and 65 years. Yet younger women can be affected too.
Family History and Genetics: Having a mother, sister, or daughter with ovarian or breast cancer roughly triples your risk. Mutations in the BRCA1 or BRCA2 genes and Lynch syndrome sharply increase lifetime risk.
Reproductive History: Your reproductive history also plays a role. Women who have never been pregnant, or who had their first child after the age of 35, may have a slightly higher risk. On the other hand, women who have had multiple pregnancies or used birth control pills for several years tend to have a lower risk. This is because each time you ovulate (release an egg), the surface of the ovary breaks and repairs itself — and frequent cell repair might increase the chance for something to go wrong.
Endometriosis:Conditions like endometriosis can also raise your risk. Endometriosis is when the tissue that normally lines the uterus starts growing outside of it, often on the ovaries. This can lead to chronic inflammation, which may increase the chance of developing certain types of ovarian cancer.
Lifestyle Factors: There are also lifestyle factors that may play a smaller role. Being overweight or obese has been linked to a slightly higher risk of ovarian cancer, possibly due to hormonal imbalances. Smoking and exposure to certain chemicals may also increase the risk, though the connection is not as strong as with other cancers.
Hormone Replacement Therapy (HRT): If taken for a long time after menopause, may slightly increase the risk. However, this depends on the type of hormones used and how long you’ve taken them. If you're using HRT, it’s best to talk to your doctor about the risks and benefits for your personal situation.
Signs and Symptoms About Ovarian Cancer
Bloating: One of the most common early signs is bloating — a feeling of fullness or swelling in your abdomen that doesn't improve. You may feel like your stomach is stretched or tight even if you haven’t eaten much. It’s more than just a little gas after a meal — this type of bloating tends to stick around and can get worse over time.
Pain or Discomfort in the Lower Belly or Pelvis: Another early symptom is pain or discomfort in the lower belly or pelvis. This can feel like cramps, pressure, or a dull ache that doesn’t seem to go away. Some women also report a heavy feeling in their pelvis or back pain without a clear reason. If this kind of pain becomes a regular issue, it’s worth checking with your doctor.
Unexplained Weight Loss: Many women with ovarian cancer also experience changes in their appetite. You might feel full very quickly when eating, even after just a few bites. Over time, this could lead to unexplained weight loss, especially if you're not trying to lose weight.
Urinary Symptoms: can also be a warning sign. You might feel the urge to pee more often or feel a sudden, urgent need to go — even if you haven't had much to drink. Some women feel like they can’t fully empty their bladder, which can be uncomfortable and frustrating.
Abnormal Vaginal Bleeding:Changes in your menstrual cycle or abnormal vaginal bleeding can also be symptoms, especially after menopause. Even spotting or light bleeding should never be ignored in postmenopausal women.
Important: If you experience these symptoms regularly or notice any unusual changes in your body, it is important to consult a healthcare professional promptly. Early detection can significantly improve treatment outcomes.
Living With and Beyond Ovarian Cancer
Survivorship starts the moment you hear “You have ovarian cancer.” It stretches through treatment, remission, and life after therapy.
- Regular follow up visits (physical exams, CA 125 tests, and scans) to catch recurrences early
- Physical rehabilitation to rebuild stamina and muscle after surgery or prolonged chemotherapy.
- Emotional wellbeing, whether through counselling, mindfulness, or support groups. Many women find strength in talking with others who have walked the same road.
- Sexual and fertility health, topics sometimes overlooked but crucial to quality of life. Options such as egg freezing before treatment and hormone replacement patches after menopause can be discussed in advance with experts like Dr Reetu Jain.
Treatment Options for Ovarian Cancer
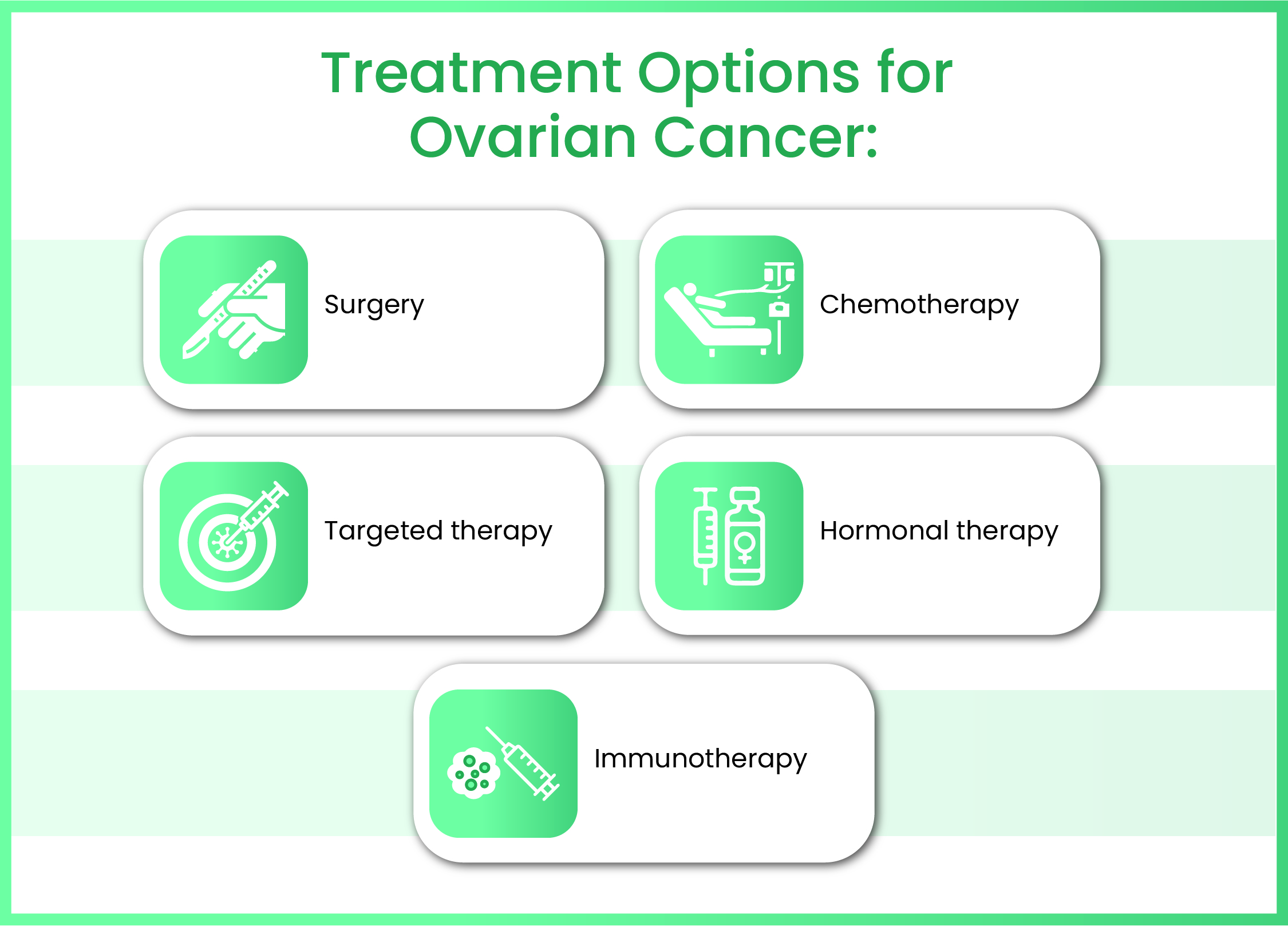
1. Surgery: For many women, surgery is the first step in treatment. The goal of surgery is to remove as much of the cancer as possible. This often involves removing one or both ovaries, fallopian tubes, the uterus (in a procedure called hysterectomy), and sometimes nearby tissues where the cancer may have spread. In early stages, surgery might remove only the affected ovary, especially if the woman wants to preserve her ability to have children. In more advanced cases, surgeons try to remove all visible cancer, which may even involve tissues in the abdomen or lymph nodes.
2. Chemotherapy: After surgery, most women go through chemotherapy, which is the use of powerful medicines to kill any remaining cancer cells. These medicines are usually given through a vein (IV) in cycles, with rest periods in between. Chemotherapy helps reduce the chances of the cancer coming back and is especially important if the cancer had already spread at the time of surgery. Some common side effects include tiredness, hair loss, nausea, and low blood counts, but these are temporary and usually improve after treatment.
3. Targeted therapy: Another newer option is targeted therapy, which uses drugs that specifically attack cancer cells without harming healthy ones. These treatments are designed to “target” the cancer’s weak spots. For example, a type of targeted therapy called PARP inhibitors is especially useful in women who have BRCA gene mutations or other specific changes in their cancer cells. These medicines can help stop cancer from growing and may be used for a longer period to keep the disease under control.
4. Hormonal therapy: Is sometimes used in certain types of ovarian cancer, especially those that are sensitive to hormones. These treatments work by blocking the hormones that help cancer cells grow. It’s more commonly used in low-grade cancers or when the disease comes back.
5. Immunotherapy: Another area of hope is immunotherapy, which helps your body’s immune system recognize and fight cancer cells. While it’s still being studied for ovarian cancer, some clinical trials have shown promising results. In the future, immunotherapy may become a regular part of treatment, especially for certain advanced or hard-to-treat cases.
Dr. Reetu Jain is a highly respected and experienced ovarian cancer specialist in South Mumbai, known for her compassionate care and advanced treatment approach. With years of expertise in treating complex gynecologic cancers, she is regarded as one of the best ovarian cancer surgeon in Mumbai. Dr. Jain combines cutting-edge medical techniques with a patient-centric approach, ensuring that every woman receives personalized care tailored to her condition and needs. From early diagnosis to long-term recovery, Dr. Reetu Jain supports her patients every step of the way, offering not just medical treatment, but also hope, strength, and reassurance. Her commitment to excellence and empathy has made her a trusted name in women’s cancer care across the country.
Frequently Asked Questions (FAQs)
A Pap test screens for cervical, not ovarian, cancer. However, pelvic exams during Pap appointments can occasionally discover enlarged ovaries that warrant further testing.
Removing both ovaries eliminates primary ovarian cancer, but a related cancer called “primary peritoneal carcinoma” can still rarely arise from the abdominal lining. Lifelong vigilance remains wise.
No, while it is more common in women over 50 and after menopause, ovarian cancer can also affect younger women. Certain types, like germ cell tumors, are more likely to appear in teens and young adults.
Ovarian cancer can return in some women, especially if it was diagnosed at a later stage. That’s why regular check-ups and monitoring are very important after treatment. However, with timely treatment and maintenance therapy, many women are able to manage recurrence effectively.
It depends on the type of treatment you had. If both ovaries and the uterus were removed, natural pregnancy is not possible. However, if one ovary was preserved or fertility-preserving methods like egg freezing were used before treatment, pregnancy may still be possible. It’s best to speak to a fertility specialist before or after treatment for personalized advice.
Eating a healthy, balanced diet with fruits, vegetables, whole grains, and protein helps your body stay strong during and after treatment. Drinking plenty of water, avoiding processed foods, and limiting sugar can also support your recovery. Always check with your doctor or a dietitian for a plan that suits your needs.


